OVERVIEW
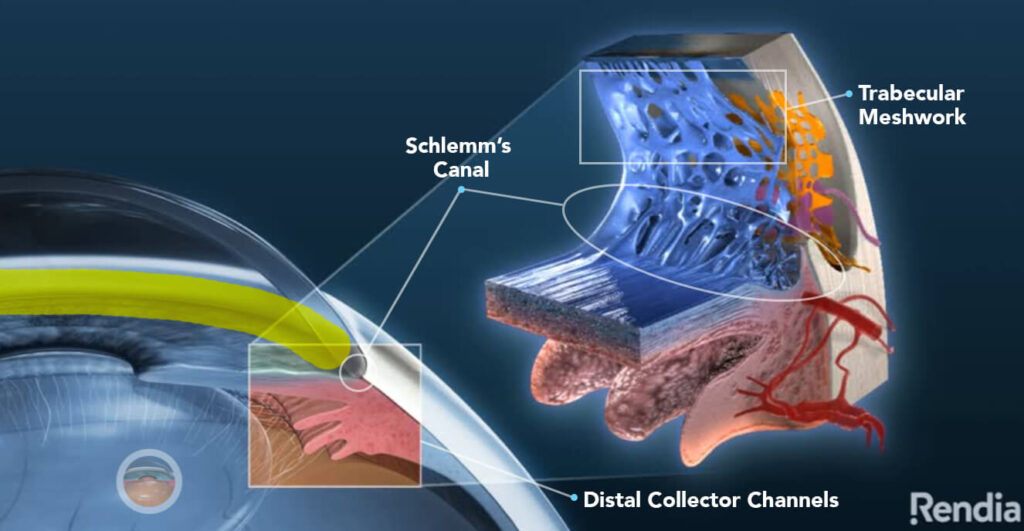
Glaucoma is a disease that can slowly destroy the delicate nerve fibers that carry signals from the back of the eye to the brain. While glaucoma typically affects people age 40 and older, it can strike at any age. Generally, high pressure within the eye is responsible for the damage, but even patients with normal pressure can experience loss of this important nerve function due to glaucoma. Glaucoma is called “the silent thief of sight” as there is no pain or noticeable change in vision during the early stages of this disease.
Most of the time, patients cannot feel high pressure or notice vision loss because it occurs from the periphery first. Therefore, patients may not take notice until it is too late. The goal of treatment is to prevent further vision loss.
Treatment needs to occur before vision is lost as optic nerve damage cannot be reversed. This is why it is important to schedule yearly eye exams. Especially if you have a family member with glaucoma as family history is the highest risk factor.